Most healthcare workers are vaccinated, but mandate fallout could still lead to cuts in services
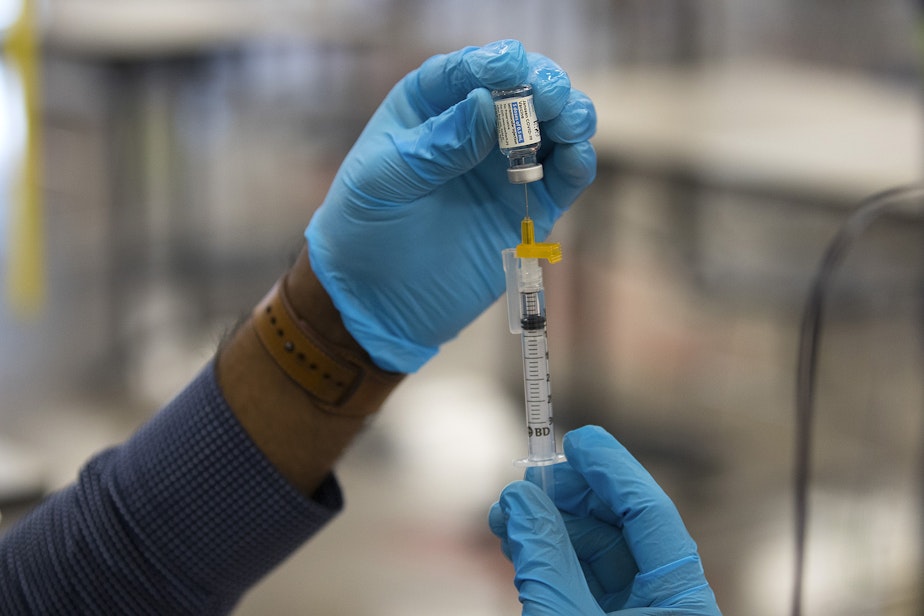
Monday marked the deadline for healthcare workers and many others in Washington state to show proof of vaccination against Covid-19, or risk losing their job under the state mandate.
Starting Tuesday, those who are unvaccinated will not be able to go to work as normal. The exception is those who have been granted an exemption for a genuine medical or religious reason and had accommodations made by their employer.
It’s still unclear exactly how many workers will lose their jobs due to the mandate.
RELATED: Unvaccinated Washington state employees face their last day on the job
Cassie Sauer is the CEO of the Washington State Hospital Association. She’s said previously that between 2-5% of hospital staff in the state could leave the workforce. That represents between 3,000 and 7,500 individuals.
However, Sauer said Monday that estimate could be high. The vast majority of hospital workers were already in compliance prior to Monday’s deadline.
Last week, the hospital association reported about 88% of workers were fully vaccinated. The remaining 12% represented a mix of people who were partially vaccinated, were in the midst of applying for an exemption, or had yet to turn in their paperwork.
Sponsored
“There has been some movement in that number,” Sauer said during a media briefing Monday.
Some people have initiated the vaccination process, others who were partially vaccinated have completed their doses, and some who were already fully vaccinated but had yet to show proof to their employer handed in their paperwork, Sauer said.
The association has not yet released updated numbers.
Over the weekend, and throughout Monday, hospitals have been scrambling to collect, and go over, final compliance records to see where they stand.
Many hospitals seem to be in good shape. On deadline day, about 98% of staff at Seattle Children’s staff were fully vaccinated, with another 1% were partially vaccinated. The remaining 1% have submitted exemptions and the hospital is working hard to accommodate and maintain as many as possible.
Sponsored
UW Medicine medical staff were 99% vaccinated, as of Monday. However, roughly 220 staff were expected to leave their positions by the end of Monday due to the mandate, according to UW Medicine chief medical officer Dr. Tim Dellit.
“And that’s impactful. It’s impactful for them, it’s impactful for their colleagues,” Dellit said.
Hospital leaders say staff losses are likely to be greatest in rural areas on the east side of the state, and state hospital association leader Cassie Sauer said personnel shortages will lead to curtailed services.
“There’s going to be caps on admissions at some rural hospitals,” Sauer said.
She said some services may potentially be closed, or longer wait times for people seeking non-emergent procedures may be seen.
Sauer said association members have felt the tension between implementing the mandate and seeing that potential staffing losses could lead to cuts to services. She said there are two important goals: get as many staff as possible vaccinated to protect them and patients, and also to keep the healthcare system functioning and serving as many people as possible.
Sponsored
"Those goals sometimes work together, and sometimes they're in conflict," Sauer said.
The mandate has increased vaccination levels and the hope is that high vaccination rates will protect against outbreaks and illness among staff in the future, preventing crippling situations.
All hospitals are trying to hire more staff she said.
Existing staffing shortages are an issue across the healthcare continuum.
Sponsored
Long term care facilities have been dealing with a lack of staff for many years, according to Washington state long term care ombudsman Patricia Hunter.
Hunter said that’s for a range of reasons, including working conditions, low pay levels, and availability of childcare. She said there were concerns that the mandate would worsen these shortages. She heard fears that facilities would close.
So far, Hunter said things are looking okay and she’s not hearing that the mandate has made things a whole lot worse.
“What we’re hoping, and what we’ve seen so far, is the vaccine mandate looks like it’s working,” Hunter said.
Sponsored
She said vaccination rates among staff are going up. As of earlier this month, about 80% of staff were vaccinated, Hunter said. She said that’s hopeful.
Hunter said prior to the mandate she was hearing concerns from residents in long term care facilities about having unvaccinated caregivers.
Nursing homes and similar settings were hit hard by Covid-19 outbreaks early in the pandemic.
Hunter said the Adult Family Home Association believes anywhere from 2-12% of workers could end up leaving the workforce because of the mandate, but only time will tell.
Hospital leaders have expressed concern about the ripple effects of staffing loss in long term care facilities, saying it will make it harder to discharge patients from hospitals that are already short on beds.
Vaccination rates and potential staff losses will vary from facility to facility. The same is true of community health centers.
The Seattle Indian Health Board (SIHB) mandated the Covid-19 vaccine for workers long before the state’s requirement was put in place. As a result, they’re now at 100% compliance according to president and CEO Esther Lucero.
Lucero said they decided from the get go they would treat the Covid vaccine like the flu shot for their staff and remove politics from the discussion. People lined up out the door to get the shots.
“As American Indian and Alaska Native people we were devastated by this pandemic. I can’t even tell you within our organization how many individuals actually have had to go to funerals,” Lucero said.
“We knew we wanted to do everything possible to protect our community.”
But not all health centers are having the same success. Pam Grindley is the chief human resources officer for the SIHB and a member of a statewide HR peer group.
Grindley said she’s hearing that there are overall high levels of vaccination among community health center employees, but the rates differ from place to place.
“Our friends on the other side of the state I think are experiencing it a little differently than we are. They’re experiencing a lot more vaccine hesitancy among their staff,” she said.
Lucero said there’s a lot of work ahead beyond the state’s vaccine mandate. Booster shots are becoming more widely available and a vaccine for younger children is expected in the coming weeks.
“Let’s not waste time with political difference, let’s just keep ourselves and our families healthy, and our community healthy, and let’s just get out of this pandemic environment,” she said.




