Why It Can Be Harder To Fight Hookworms In Alabama Than In Argentina
This story definitely has a yuck factor.
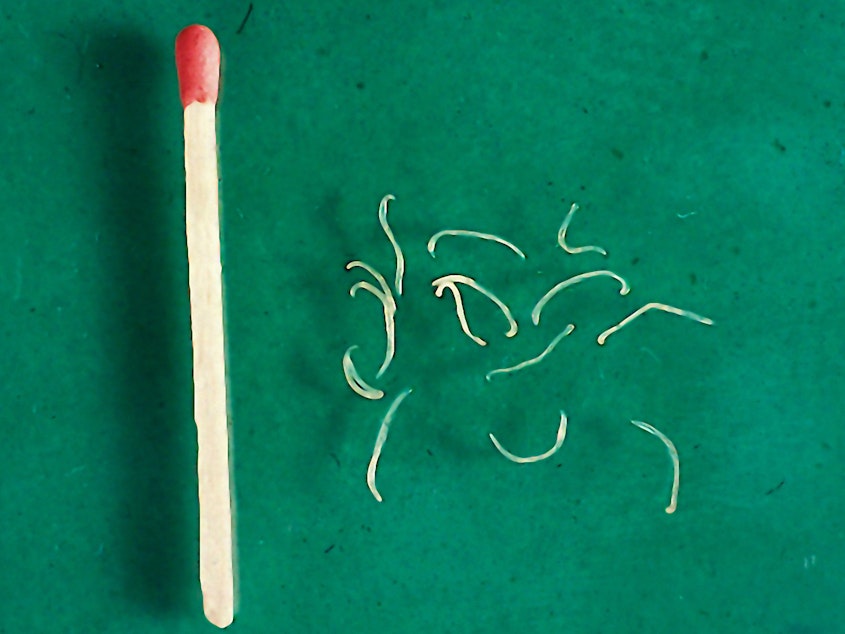
It's about hookworms.
When hookworm eggs land on moist, warm ground, via human feces, they develop into larvae, raise their tiny selves upward, and wave back and forth, looking for bare feet to latch onto. The parasites penetrate the skin, enter the bloodstream, and eventually migrate to the small intestine — where they settle in, mature and start sucking blood and laying eggs. When the worms and their eggs are passed in a host's stool, the cycle begins anew.
Hookworm disease flourishes in hot, moist climates where people have limited access to water, inadequate sewage systems and poor hygiene.
There are ongoing efforts to wipe it out in Africa. Latin America. Asia.
Sponsored
And now, in Alabama.
Dr. Rojelio Mejia, infectious disease specialist at Baylor College of Medicine, says the parasites are no strangers to U.S. soil. In a paper published in 2017, Mejia and his team reported finding more than a third of the people in one Alabama county were infected with hookworm disease.
Dr. Rojelio Mejia, infectious disease specialist at Baylor College of Medicine, says the parasites are no strangers to U.S. soil. Mejia and his team have found that more than a third of the people in one Alabama county were infected with hookworm disease.
Mejia has worked to quell hookworm disease in Ecuador, Mozambique, the grassy plains of northern Argentina, and now, he and partners are leading efforts to control the outbreak in rural Alabama. We talked with him by telephone about the disease and the various struggles the U.S. has keeping it under control compared to resource poor countries. His answers have been lightly edited for space.
What does hookworm need to thrive?
Sponsored
It's a really fragile parasite. It needs moist, loamy soil — the same type of soil found in Alabama, the plains of Argentina and other places with hookworm. It needs a tropical or sub-tropical climate. And it requires poor sanitation conditions where human waste gets into the soil.
How long has hookworm been in the U.S.?
Public health people have talked about hookworm the 1800s. In the 1900s, a study in some counties in Alabama found about 60 percent of people had hookworm — mostly African-Americans and poor whites. The sharecropper was the classic presentation. The Rockefeller Foundation funded a project to try to eradicate hookworm, and studies in the 1950s, showed the infection rate was about 40 percent, not just in Alabama, but throughout the South. But in recent years, because interest had apparently waned, hookworm studies in the U.S. disappeared off the radar.
Until I came on the scene in 2013.
So what can of worms did you open in 2013?
Sponsored
We studied rural Alabama and found about 35 percent of people in one county are infested with hookworm. We chose Lowndes County because it previously had a high rate of hookworm, continues to have a high rate of poverty, and many residences have open sewage systems. (The study, "Human Intestinal Parasite Burden and Poor Sanitation in Rural Alabama," was published in October 2017, in American Journal of Tropical Medicine )
Is hookworm found anywhere else in the U.S.?
The only recent human studies have been done in Alabama. But soil and conditions can be similar in parts of Texas, Louisiana, Mississippi and South Carolina. We assume conditions are right in much of the Southeast U.S., but urban areas will have very little because of paved driveways, cement floors and sidewalks, while rural areas will have more.
What are the symptoms and long-term consequences of hookworm infection?
There's a little bit of a rash where the worm entered. The worm travels to the lung, and some people can get pneumonia. There's some evidence that it can contribute to asthma. When it's in the small intestine, it can cause diarrhea. The most serious problem is anemia, because the worms are voracious consumers of red blood cells.
Sponsored
Can poor countries offer any pointers to the U.S. in handling hookworm?
How do they handle it in poor countries? They don't handle it. They're overwhelmed. They try, but their hands are tied by poverty.
But one thing they do with great efficiency is give albendazole, a drug used to treat hookworm. I was in Argentina at a school, and they had all the kids line up for treatment. They took it in front of us.
It's mass drug delivery. They go into a school, and they don't even test for hookworm. The problem is so great, they assume most kids are infected, and they get automatic treatment twice a year.
In the U.S., we're more independent thinking. Can you imagine going anyplace in the U.S. and saying, "Your kids have to take this tablet." It wouldn't fly!
Sponsored
Was the treatment the kids in Argentina got effective?
Yes, but then they go back home. In three or four months, all of them are re-infected. That's the problem. It's a band-aid on a major health problem.
If we could provide better sanitation systems, we could curb the infection rate, but there's not enough money to pay for septic systems in many parts of the world.
Are there disadvantages to being diagnosed with hookworm in the U.S. compared to poorer countries?
One disadvantage in the U.S. is the cost of treatment. In Columbia, we treated 400 patients with albendazole for pennies per patient, thanks to a donation from Mark Cuban, owner of the Dallas Mavericks. But in the U.S., the cost is astronomically higher — up to $500 a pill. If you don't have insurance, the cost is prohibitive.
One disadvantage in the U.S. is the cost of treatment. In Columbia, we treated 400 patients with albendazole for pennies per patient, thanks to a donation from Mark Cuban, owner of the Dallas Mavericks. But in [most places in] the U.S., the cost is astronomically higher — up to $500 a pill. If you don't have insurance, the cost is prohibitive. [But in rural Alabama, thanks to a new collaboration between researchers at the National School of Tropical Medicine at Baylor College of Medicine and the Mark Cuban Cost Plus Drug Co., children with hookworm infection will receive the drugs at greatly reduced cost.]
Another disadvantage in the U.S. is diagnostics. In Ecuador, they know what a parasite looks like under a microscope. In the U.S., because hookworm is rare, physicians, who won't know what to look for, could miss it.
Are there unique difficulties in doing research in poor, rural areas of the U.S.?
There's a problem of centuries of mistrust of the healthcare system in rural America — especially among African-Americans. I had a plan to do 100 stool samples from 100 people. I only got 11. They were wonderful people. They invited us in and gave us glasses of Tang. But no one wanted to give us a stool sample. Finally, we got 60 samples because a community organizer, Catherine Flowers, helped us. They knew her and trusted her, and we got the samples. [Catherine Flowers, author of Waste: One Woman's Fight Against America's Dirty Secret, was a MacArthur fellow in 2020 and is an environmental health researcher.]
We also had a lot of pushback from public health departments because they wanted to deny the problem. It can't be us! We're the United States! I understand that it's embarrassing. It's all about poor sanitation, about poverty. In Alabama, it's illegal not to have a septic system. But many people who live in the poorest areas can't afford a septic system.
Without a septic system, what happens when people flush the toilet?
People do what's called straight piping for sewage, running a large pipe as far away from the home as possible. All the sewage goes through these pipes to a ditch or a landfill. But it's hilly and it rains, so the hookworm eggs end up getting spread throughout the environment.
The same thing is true in Colombia and Honduras and a lot of poor countries. There, they use outside latrines and outhouses, but it all ends up getting into the soil.
Treatment works — but only temporarily until people get re-infected. So what's the answer?
It's a sanitation problem and the solution is adequate sanitation systems. It's going to take not just physicians and scientists to fix it. It's going to take engineers, and politicians who say that we need money for this.
Susan Brink is a freelance writer who covers health and medicine. She is the author of The Fourth Trimester and co-author of A Change of Heart. [Copyright 2021 NPR]



